|
|
|
|
| |
| You Are Here: Home > Recently Diagnosed > Treatment Choices > Clinical Trials |
|
Treatment Choices: Clinical Trials |
|
|
Overview:
Clinical trials are research (experimental) studies in people. Federal laws require all new drugs, diagnostics, imaging and surgery techniques that are used in people to be tested in a standardized setting. This standardized setting is called a clinical trial (study).
We are discussing clinical trials in the treatment section because as research moves out of the laboratory and into people, some patients have the option of entering a clinical trial rather than receiving standard of care. We will discuss all aspects of this option in this section so you can better understand how this may fit into your treatment choice decision.
The process from the very beginning of looking for a new therapy until it becomes a standard treatment takes many years and goes through many steps and phases. This entire process is referred to as research.
Research Steps:
- Preclinical Step (in the laboratory)
- Lab bench phase (cell cultures and sometimes referred to as “in vitro”)
- Lab animal phase (referred to as “in vivo”)
- Clinical Trial Step (in humans)
- Phase I: Is the treatment safe?
- Phase II: Does the treatment work? (is it effective)
- Phase III: Is the treatment more effective than standard choices?
- Phase IV: Continue to monitor for effectiveness and safety.
The most important piece of information for you, as a patient, is that you may be eligible to enter a clinical trial when you are newly diagnosed, or if your cancer returns at a later date.
Always ask your doctor if you are eligible for a clinical trial. If you are eligible, be sure to discuss the benefits versus the risks of entering the trial.
|
|
|
|
| |
| |
Pre-Clinical Basic Research Step :
Question: How are new drugs/therapies discovered?
Answer: Through Laboratory Research.
|
| |
 |
Before testing new approaches in clinical trials that include people, extensive pre-clinical research is conducted.
Laboratory: Occurs in the laboratory through testing in cell lines and tissues. See picture.
Animals: Research moves from test tubes into animal models. |
|
| |
Tests in animals analyze a drug’s chemical properties and toxicity. Since the way that drugs react in animals is different from how they affect humans, animal testing is a preliminary step in the research process.
Results from laboratory research must demonstrate that the new intervention is likely to be safe and has a significant chance of being effective before trials are done in people.
Most cancer research studies are conducted in a progressive series of steps called phases.Progression to the next phase requires success related to the research goal with the benefits being greater than the risks they present to patients.
The following describes the most common purposes and characteristics for each phase of a clinical trial.
Clinical Trial Research Steps:
Question: What happens after new therapies are tested in the laboratory with enough preliminary evidence for evaluation in people?
Answer: Clinical trials in people are conducted.
This research occurs after laboratory research shows promise in animals. When research moves to people, it is called a clinical trial. This is still research as the effectiveness is not yet known.
• Phase I Clinical Trials: The first time the new intervention (drug, surgery etc) has ever been tried in people.
- Number of people: small number (15-30)
- Location of Clinical Trial: usually just one place
- Purpose of Phase I Trials:
- Identifying the safest dosage or intervention:
Sometimes the dosage is gradually increased in new patients where the first few patients receive a lower dose than those admitted later in the study.
- How the dose or intervention effects People: Exploring how the intervention is processed by the human body and how it influences functions in organs.
- Decide when and how to give the dose or intervention: Assessing when and how the therapy is safest when given to people such as once per week versus once every two weeks, and larger dosages all at once versus smaller dosages given over time.
- Time Frame: Several months.
CISN TIP:
Phase I trials carry the most risk as it is the first time the intervention is being tested in humans. Further, in phase I drug trials few patients will receive a drug dose high enough to be of benefit.
Discuss the risks and benefits carefully with your doctor.
• Phase II Clinical Trials: Begin to assess whether or not the intervention is considered effective. Researchers also continue to collect information about how the approach works in people and what side effects it produces over longer periods of time.
- Number of people: small number (less than one hundred)
- Location of Clinical Trial: more places (~1-10).
- Purpose of Phase II Trials:
- Is the intervention effective?
Document effectiveness.
- How does the dose affect people?
Continue to gather data on how the drug effects the body.
- Time frame:
Can take more than a year to complete.
• Phase III Clinical Trials: Compare the effectiveness of the new, experimental approach with standard care.
- Number of people: larger number (up to several thousand)
- Location of Clinical Trial: many places (up to several hundred)
- Purpose of Phase III Trials: To compare the intervention against the standard of care, is it as good as.
- Time Frame: Can take at least 3 years and even up to 10 years to complete.
Characteristics of Phase III Trials:
|
| |
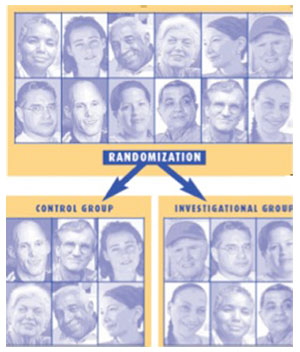 |
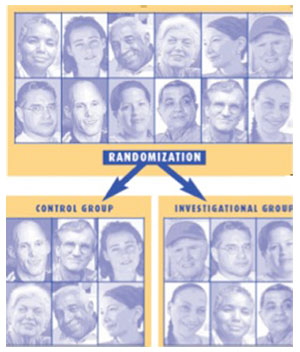
Treatment assignment to either the new, experimental approach or standard care (control group) occurs through a process called randomization.
Patients are assigned to a study treatment group by a computer. Randomization occurs to ensure that unknown factors do not influence study results. |
|
| |
To further reduce the possibility of bias, these studies can also be blinded where the study treatment assignment is not identified to patients, doctors or research investigators.
A placebo, (an inactive substance) or the standard treatment will be given to half of the study participants. They will be compared to the other half of the study participants who will receive the new investigational treatment.
Placebos are rare in cancer trials and only given when investigators need to make all study treatment groups appear the same, or when no effective treatment is known for a disease.
Trial endpoints or outcomes, measure the intervention’s potential effectiveness. I n Phase III studies endpoints often evaluate survival, tumor reduction, symptom relief, or quality of life.
• Phase IV Clinical Trials: In addition, after a treatment has been approved and is being marketed, the drug's maker may study it further in a phase IV trial. The purpose of phase IV trials is to evaluate the side effects, risks, and benefits of a drug over a longer period of time and in a larger number of people than in phase III clinical trials. Thousands of people are involved in a phase IV trial.
|
| Summary of Clinical Trial Phases: |
Phases of Clinal Trials
Trials take place in different phases, each designed to answer different research questions. |
| |
Phase I |
Phase II |
Phase III |
Phase IV |
| Number of Participants |
15-30 people |
Less then 100 people |
Generally 100 to thousands of people |
Several hundred to several thousand people. |
| Purpose |
To find a safe dosage
To decide how and agent should be given
To observe how the agent affects the human body |
To determine if the agent or intervention has an effect on a particular cancer
To see how the agent or intervention affects the human body |
To compare the new agent or intervention (or new use of treatment) with the current standard |
To further evalutate the long-term safety and effectiveness of a treatment |
|
| |
The trial phases are explained in the context of drug treatment trials, but the concepts apply to most types of clinincal trials.
Types of Clinical Trials:
Treatment Trials: Study investigational (new) drugs, new-targeted therapies, biologics, surgical procedures, radiation and other potential therapies.
Screening Trials: study ways to detect cancer earlier or more easily. |
| |
 |
They are often conducted to determine whether finding cancer before it causes symptoms decreases the chance of dying from the disease.
These trials often involve people who do not have any symptoms of cancer. |
|
- Diagnostic Trials: study tests or procedures that could be used to identify cancer more accurately. Diagnostic trials usually include people who have signs or symptoms of cancer.
- Prevention Trials: study interventions such as drugs, lifestyle modification, complementary and alternative therapies, and other approaches that might reduce the risk of getting cancer.
- Quality of Life Trials: (also called supportive care) explore ways to improve the comfort and quality of life of cancer patients and cancer survivors. These trials may study ways to help people who are experiencing nausea, vomiting, sleep disorders, depression, or other effects from cancer or its treatment.
Possible benefits of being in a clinical trial:
|
| |
 |
Clinical trials typically offer high-quality cancer care. If you are in a randomized study and do not receive the new treatment being tested, you will receive the best known standard treatment. This may be as good as, the same as, or better than, the new approach. |
|
| |
- If a new treatment is proven to work and you are taking it, you may be among the first to benefit.
- By looking at the pros and cons of clinical trials and your other treatment choices, you are taking an active role in a decision that affects your life.
- You may be more closely monitored so that any side effects that may arise can be found early.
You have the chance to help others and improve cancer treatment for future patients. Every treatment that you may be offered had to pass through the clinical trial system so you are benefitting from someone else’s participation. By enrolling in a clinical trial, you can continue building on the scientific knowledge that contributes to the discovery and use of new, better treatments for future patients.
Possible risks or drawbacks of being in a clinical trial:
- New treatments under study are not always better than, or even as good as, standard care.
- If you receive standard care instead of the new treatment being tested, it may not be as effective as the new approach.
- New treatments may have side effects that doctors do not expect or that are worse than those of standard treatment.
- Even if a new treatment has benefits, it may not work for you. Even standard treatments, proven effective for many people, do not help everyone.
- Health insurance and managed care providers do not always cover all patient care costs in a study. What they cover varies by plan and by study. To find out in advance what costs are likely to be paid in your case, check with your insurance company and talk to a doctor, nurse or social worker from the study.
- You may be required to have more tests and/or doctor visits.
Eligibility:
Very specific criteria are used to see if you qualify to enter into a clinical trial. Because clinical trials are research studies, doctors must be sure that they compare people who are very similar so they can report results that are scientifically and statistically accurate.
Inclusion Criteria: You must meet specific requirements to enroll. They are often related to specific aspects of your cancer as well as other aspects of your health.
Exclusion Criteria: These specific criteria will prevent you from entering the trial.
Questions to ask your Doctor if you are
Considering a Clinical Trial:
- Why is the trial being done?
- Why do doctors who designed the trial believe that the treatment being studied may be better than the one being used now? Why may it not be better?
- How do the side effects (short/long term; minor/serious) compare to standard of care?
|
| |
 |
- What are the risks and benefits of participating in the trial and all of your other choices?
- How long will I be in the trial?
- What extra tests and procedures are required?
- How would the trial affect my daily life?
|
|
| |
- Will I have to travel farther and/or to different places or more frequently if I am in the trial?
- Will I have to pay for any treatment or tests?
- Does the trial include long-term follow-up care?
- How does the treatment I receive in this trial compare to other treatment choices in terms of possible outcomes, side effects, time involved, costs to you and quality of your life?
Informed Consent Process:
If you are eligible and decide to enter a clinical trial you will be asked to sign a consent form. This is the last step before entering a clinical trial. We will discuss the steps before and after the consent document briefly here and in more detail in the research section.
Step 1: Discuss clinical trials with your doctor:
- Be sure to ask your doctor to compare the risks and benefits of your standard of care options with any clinical trials for which you may be eligible.
- Take the consent form home and discuss it with your support team. With their help, prepare a list of additional questions or concerns to discuss with your doctor or medical team.
Step II: Determine eligibility:
- Your treatment team will do this for you. If you find the trial online, bring the information to your doctor.
Step III: Sign a consent form:
- Prior to signing the consent form, raise all of your questions and concerns with your health care team.
- Be sure that you understand all of your options, what phase the study is, what extra procedures you may have, any extra costs you may incur. Etc.
- You may be asked to donate tissue. This is a very important donation that you can make. Researchers will use this tissue (always a very small amount) to help them find better, more effective treatments. Read more about the importance of tissue donation in our research section.
Step IV: Be closely followed and receive updates on trial results. One of the benefits of being in a clinical trial is that your doctor will closely follow you. It is important to take all drugs as prescribed, to have all extra tests or procedures and to report any side effects or concerns with your health care team.
Finding Clinical Trials
Overview
Cancer Cooperative Groups, the NCI, Cancer Centers, Drug Companies, Hospitals and local Doctors conduct clinical trials. |
| |
 |
The NCI, Drug Companies, Philanthropic Organizations and other groups may fund them. They take place in many diverse places all over the Country and abroad.
When trying to locate a clinical trial it is important to remember that no single resource, including those from the NCI, lists every cancer clinical trial. |
|
| |
CISN Tip:
Always ask your Doctor if there are any clinical trials for which you are eligible for. You may decide not to enter a clinical trial, but you should have the opportunity to consider this option as part of your treatment process.
Reminder: Clinical trials are research studies to find better treatments, diagnostics, prevention strategies, surgery and imaging techniques.
They may be:
Better than, the same as, or worse than standard of care.
Your Guide to Finding Clinical Trials:
Remember not all trials are listed or can be found in one place. |
| |
| Coming Soon ... |
| |
|
|
| |
|
|
|
| |
|
|
| |
| Copyright © 2006-2021 CISN - All Rights Reserved. |
| |
| Site Design by: Cara M. Caloroso |
| |
|